We are really excited to have Karyn from Adelaide based Head2Toe First Aid on board here at Kids in Adelaide to write us some really useful, interesting and important health and first aid articles for our website. Karyn is an Adelaide based, Registered Nurse and Trainer with 18+ years of experience dealing with the medical and first aid needs of both adults and children. She is also a Mother and has firsthand experience dealing with Asthma and Allergies/Anaphylaxis on a daily basis. These roles enable Karyn to both appreciate the first aid challenges that a Parent/Caregiver can face, and understand the importance of quality first aid training in the community. Karyn’s Facebook page has some really great info on it so pop over and say hello!
Please note: this article was written for information and education purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read in this article.
In Australia, an astounding 1 in 10 babies born, will develop food allergies, making allergies one of our fastest growing chronic medical conditions. Whilst medical research is promising both in Australia and Worldwide, currently there is no cure. Our best defence to help protect people with allergies is through raise community awareness and understanding. As a Nurse, a First Aid Trainer and a Mother of a child with multiple food allergies and anaphylaxis, allergy education is something that I am passionate about.
Allergy diagnosis can be an overwhelming time for a family. Often the diagnosis is preceded by either a dramatic event or a stressful time of concerning symptoms which can fuel the overwhelming feeling. The more people that understand allergies, the more support that there will be for people during as this intense period of “learning to manage allergies” starts.
In today’s world, the word allergy is fairly commonplace. However, not many of us fully understand what allergies are. So, let’s look at the “what” of allergies a little deeper to help us understand when, and how to treat allergies and anaphylaxis….
Allergies and anaphylaxis explained
An allergy occurs when the body’s immune system reacts to a substance that for other people is harmless. This substance is called an allergen and is what triggers the allergic reaction. Anaphylaxis is the most severe and life-threatening form of an allergic reaction.
Common examples of allergens are dairy, egg, nuts, soy, wheat, seafood, sesame and shellfish. The majority of allergies are not severe and many children will grow out of allergies (often dairy by approx. 5 years and egg by 7 years). However, nut, sesame, fish and shellfish allergies are more likely to be lifelong.
As mentioned an allergic reaction occurs when a person is exposed to their allergen (what they are allergic too). This exposure could be ingestion (eating), touch, inhalation (e.g. pollens) or injection such as a bee-sting or medication.
Symptoms…. Allergy vs Anaphylaxis
Once a person has been exposed to their allergens they may develop symptoms that make you aware they are having an allergic reaction. These symptoms may differ with each exposure and with each allergen.
We know that a person with an allergy is more likely to have an anaphylactic reaction if they also have poorly controlled Asthma. There are also other variables that can influence how the allergic reaction presents itself such as:
- Illness: if the person is sick their immune system is already busy and the reaction maybe worse
- Exercise: running around can speed up the reaction
- Amount: the amount ingested
- Heat: heating food changes the protein structure. People are often able to tolerate an allergen (e.g. dairy) in a baked form before a raw form.
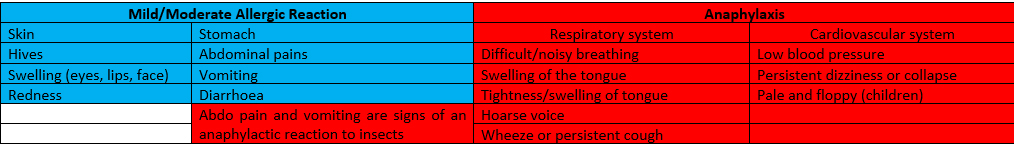
Symptoms differ between a mild/moderate allergic reaction and anaphylaxis (severe/life threatening). Currently the best defence and management for allergies is risk management and avoidance of the allergen in addition to raising community awareness.
Generally speaking, a mild/moderate reaction involves the skin and stomach (except in an insect allergy see below) whereas a life threatening anaphylactic reaction may involve the skin and stomach but always involves the respiratory system (breathing/airway) and/or the cardiovascular system (heart and blood vessels).
EpiPen, don’t delay! What you need to know.
If you think about the majority of the mild/moderate symptoms, with the exception of the abdominal symptoms they all occur on the outside of the body and involve swelling, itching and redness. These symptoms are all controlled by a chemical released called histamine. The vomiting is the body’s very clever way of getting rid of an allergen that may have been ingested. Following the Action plan (attached below) we can see that the important steps in a mild/moderate reaction are to remove the allergen, stay with the person, administer any antihistamine prescribed and locate their EpiPen in case the symptoms worsen.
In contrast anaphylaxis symptoms involve the heart and lungs/airways. Both are essential for life and so any symptoms of anaphylaxis, even a simple cough, in the context of a possible exposure to an allergen should always be treated with adrenaline (EpiPen).
A simple way of thinking about it is… Anaphylaxis is controlled by a “party of chemicals” that take over the body. Just like any good party it can get out of hand easily as every chemical brings along a chemical “friend.” The key to controlling an anaphylaxis party is to stop it at the first sign no matter how subtle. The chemicals involved in anaphylaxis are NOT histamine and so a simple anti-histamine will not work in anaphylaxis. The only medication that will work on anaphylactic chemicals, is adrenaline (an EpiPen). This MUST be given without delay before the cascade of anaphylaxis chemicals take over, dropping a person’s blood pressure and making anaphylaxis very difficult to treat.
Here is a copy of an anaphylaxis action plan which goes through the symptoms and steps
But simply put, at the first sign of anaphylaxis:
- Lie the person down (or sit with feet out if breathing trouble)
- Give the EpiPen (firm fist, blue to the sky, orange to the thigh, hold for 3 secs, then needle out and a needle sheath covers the needle automatically). Note the new time of 3 secs for administration and the removal of the massage step.
- Call the ambulance. Everyone who has had an EpiPen must be monitored in hospital even if a complete recovery. There is a chance of a rebound reaction when the EpiPen wears off.
- A further EpiPen maybe needed after 5 mins if symptoms still present.
- Start CPR if unconscious and not breathing
- Remember an EpiPen is unlikely to do any harm even if it was not anaphylaxis so if in doubt give the EpiPen
People with allergies often develop very good body awareness at an early age. Sometimes before they can put words to what is happening. Trust people with allergies when they think they are reacting, DO NOT force them to eat food that they say make them feel funny. We gave my son the words his “alarm clock” as he often describes a tingle in his mouth or a mouth feeling. He now says “mum my alarm clock is going off.” That combined with us watching his reactions during food challenges in hospital has made us confident that he is very aware of a reaction before we can measure it with hives or anything more sinister. Encourage that very precious knowledge of their body and don’t question it. Help people with allergies trust their instinct, it may save them.
This basic knowledge of allergies and anaphylaxis lays the foundation to help you better understand the needs of a person with allergies. Even if you or your child does not have allergies, with 1 in 10 people developing allergies, chances are you or your child will know someone with allergies now or in the future. Learn in my next article how you can help someone with food allergies feel comfortable coming to your house or attending your child’s party.